Outline
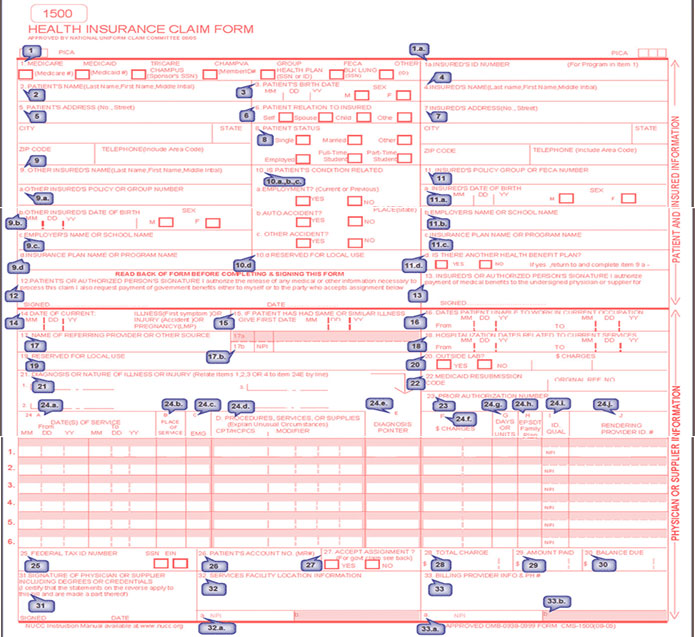
The CMS-1500 claim form serves as a means to submit non-institutional claims for healthcare services to a variety of private insurance providers, as well as to Medicare, Medicaid, and various government health insurance programs.
Form CMS-1500 is the established paper-based claim form used for billing Medicare Fee-For-Service (FFS) Contractors in situations where a paper claim submission is permissible.
The 1500 form was created and is maintained by the National Uniform Claim Committee (NUCC), and it is also known as CMS-1500. According to CMS, non-institutional providers can use this form to bill Medicare carriers. It is also used for billing Medicaid State Agencies.
Originally, this form was designed for providers to submit claims for payment to government insurance payers. Today, it is also a regular form used by private payers. This form's digital counterpart is 837 EDI. This form should be used anytime a payer is needed to submit a claim, either manually or digitally.
CMS-1500 Fields - A Complete View
Let's break down the CMS 1500 sample form step-by-step with a field number, covering each field in detail. Refer to the tabular form below.
Note: Every detail in the section must be accurate, or the claim will be denied.
| Field Number | Explanation |
|---|---|
| 1 | Payer Type - Check off the type of insurance you plan to submit the claim to. |
| 1.a | Patient Insured's ID Number |
| 2 | Patient's Name (Last, First, and Middle Initial) |
| Type 6 | Benefits from Medicare, Medicaid, and Medi-Cal are extended to HMOs.Healthcare providers cannot submit bills directly to Medicare. Note that the patient can cancel the HMO anytime to get back to coverage Type 5 (Active on the 1st of Next Month) |
| 3 | Patient's DOB and SEX |
| 4 | Insured's name. (This name might be different than the patient's name if they are on a family member's plan) |
| 5 | Patient address, city, state, zip code, & home phone number. |
| 6 | Patient's Relationship to the Insured |
| 7 | Insured person's information like address, city, state, zip code, & phone |
| 8 | Patient's marital status, employment status, & student status |
| 9 | Name of the Insured Person [if the claim is for primary insurance, the other payer is secondary insurance, similarly if claim is for secondary insurance, the other payer is primary insurance and if claim is for tertiary insurance, the other payer is secondary insurance] |
| 9a | Other insurance group ID |
| 9b | Insured person's DOB and SEX of other payer |
| 9c | Employer name of the other payer insured person |
| 9d | Name of Other Payer/ Other Insurance plan name |
| 10 | Is the patient's condition related to one of these items? |
| 10a | Their employment? Check yes or no |
| 10b | An auto accident? Check yes or no |
| 10c | Another type of accident? Check yes or no |
| 10d | Reserved for local use |
| 11 | Group ID of destination payer |
| 11a | Insured person's DOB and SEX |
| 11b | Insured person's employer's name |
| 11c | Name of the Destination Payer/ Insurance plan name |
| 11d | This will be YES if there is multiple payers for the patient in the Patient Master, and NO if there are no other payers for the patient. |
| 12 | Patient's or authorized person's signature |
| 13 | Insured's authorized person's signature |
| 14 | Onset date of current illness or accident date or date of pregnancy |
| 15 | First date of similar illness |
| 16 | Date patient unable to work in current occupation |
| 17 | Name of referring provider |
| 17b | NPI# of the referring provider |
| 18 | Admission/hospitalization date From & To |
| 19 | Reserved for local use |
| 20 | Were lab services rendered? Check yes or no. Include dollar amount, no commas, decimal points, or dollar signs. |
| 21 | Diagnosis code. Include the number 0 in the right corner to indicate that you are utilizing ICD-10 codes. Sections A-L - use ICD-10 codes to indicate the "sign, symptom, complaint, or condition" as it relates to the services you provided. |
| 22 | Medicaid resubmissions code |
| 23 | Prior authorization number |
| 24a | Date of Service – From & To |
| 24b | Place of Service Selected |
| 24c | Was this an emergency? Check yes or no |
| 24d | Enter CPT code for billing along with modifiers |
| 24e | Diagnosis code references letters |
| 24f | Dollar amount being billed with CPT code |
| 24g | Number of units being billed against CPT code |
| 24h | This section varies by the payer. Was this covered under a state plan? Respond accordingly. |
| 24i | Secondary ID type qualifier for the rendering provider against the billed insurance - The type of provider identification number you are using and the corresponding modifier |
| 24j | Secondary ID for the rendering provider against the billed insurance - The number that corresponds to the modifier in the previous section along with your NPI |
| 25 | Employer ID or SSN of the billing provider |
| 26 | Patient account number |
| 27 | Do you accept assignments under the payer’s terms? Check yes or no |
| 28 | Total Charge for this claim |
| 29 | Total Amount Paid for this claim |
| 30 | Total Balance Amount for this claim |
| 31 | Rendering provider name, signature on file & claim date |
| 32 | Service location details selected in this claim |
| 32a | NPI Number of the selected Service Location in the claim |
| 33 | Billing Provider Information |
| 34 | NPI Number |
| 33b | Secondary ID type qualifier & Secondary ID for the rendering provider against the billed insurance |