How to check Eligibility and Benefits using Medi-Breeze Portal
Here's a simple guide on how to check Eligibility and Benefits using the Medi-Breeze Portal:
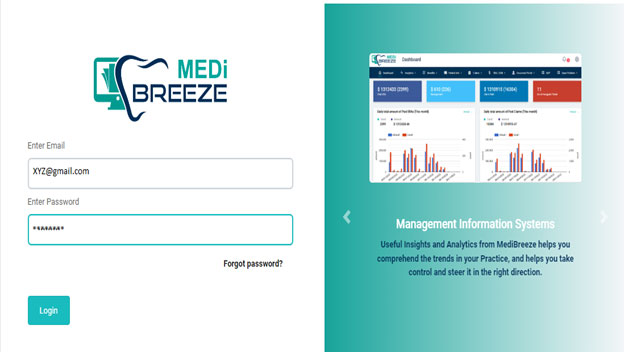
Step 1: To begin, log in to the Medi-Breeze site using the login credentials shown below.
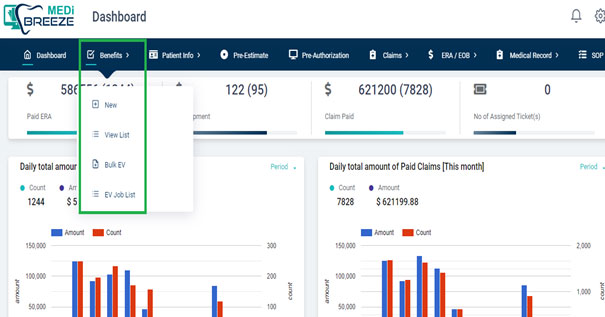
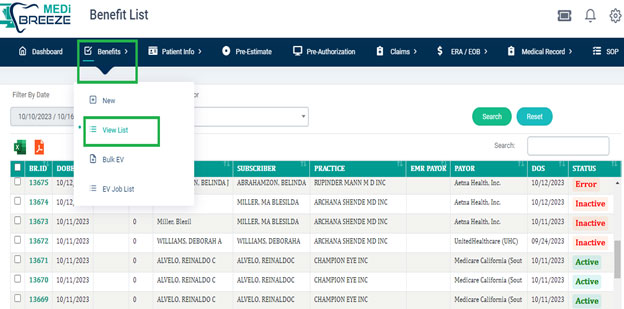
 Step 2: After you've successfully logged in with your credentials, simply head to the top of the portal and click on the "Benefits" tab. There, you'll discover a range of options that include creating a New Eligibility, accessing a List of Eligibility, managing Bulk EV, and checking out the EV Job list. You can take a look at the screenshot provided below for your reference.
Step 2: After you've successfully logged in with your credentials, simply head to the top of the portal and click on the "Benefits" tab. There, you'll discover a range of options that include creating a New Eligibility, accessing a List of Eligibility, managing Bulk EV, and checking out the EV Job list. You can take a look at the screenshot provided below for your reference.
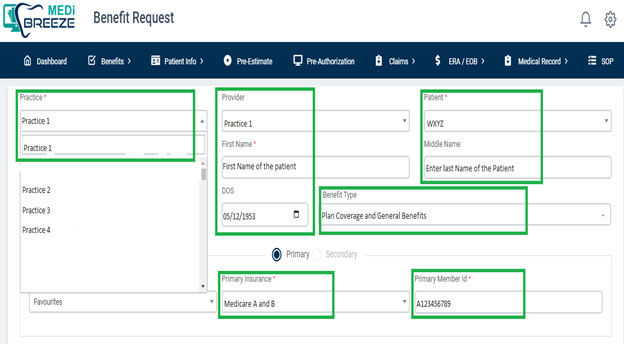
Step 3: When we generate a New Eligibility, we'll be able to view the detailed information as shown below.
Step 4: Once you've filled in the required fields, which are highlighted in green, and clicked the submit button, you'll be directed to a screen displaying a list of patients and their existing benefits. In other words, by selecting the "view list" option, you can easily access all the eligibility information for each patient in one place, as displayed below.
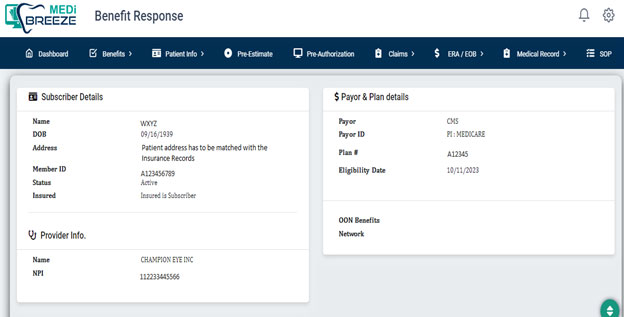
Step 5: When you select the “Active” in the “Status” column, you'll gain access to comprehensive details about each patient's benefits. This information includes the patient's name, date of birth, address, member ID, and their coverage status, whether it's currently “Active” or “Inactive.” It's crucial to pay attention to the patient's effective date and end date. If the coverage has expired, it's important to communicate with the patient to discuss extending their coverage or to check if they possess another insurance card with active coverage. In such cases, the alternative card's eligibility is verified, and the appropriate steps for further assessment are taken.
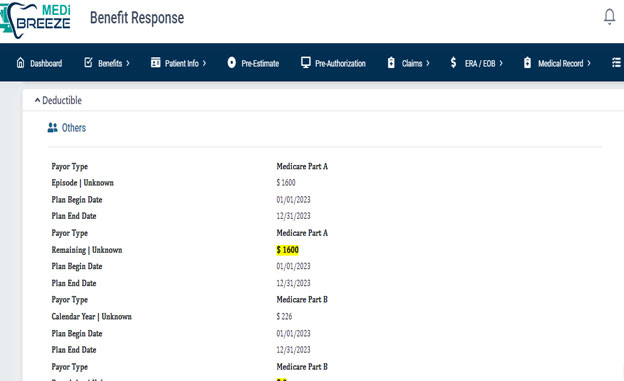
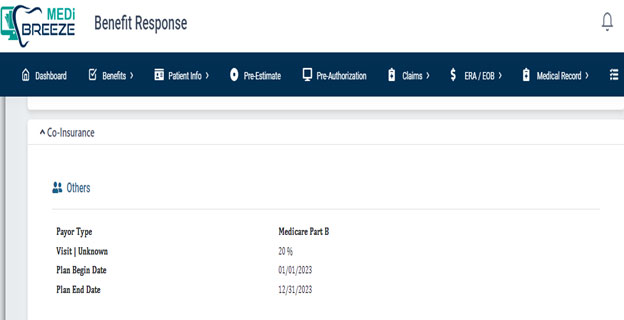
Step 6: On selecting the “Expand All” tab, you can find information about the patient's insurance plan type, whether it's a PPO plan, HMO plan, or any other type of insurance plan. It's essential to click on the “Additional Benefits” section to verify that the information we've gathered for our process is accurate. For better clarity, refer to the below screen shots.
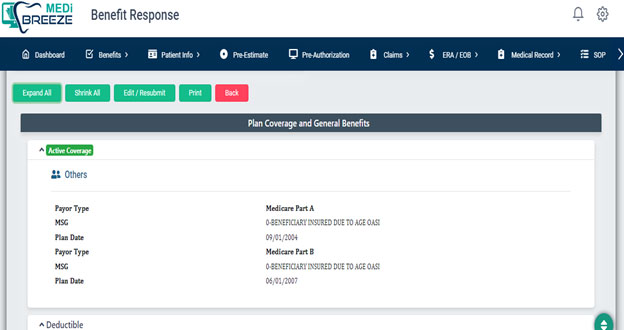
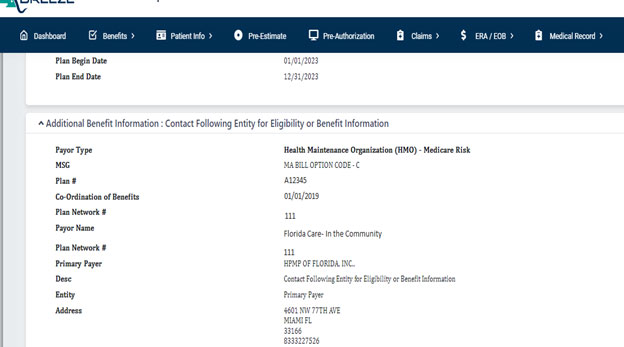
Note: If the patient is enrolled in a Medicare HMO or a general HMO plan, it is not possible to proceed with their treatment. In such cases, the patient will need to cancel their HMO plan and switch to either a Supplement or a PPO plan to be eligible for Medicare benefits. We will be able to process Medicare PPO and general PPO plans, as well as various other commercial insurance types.